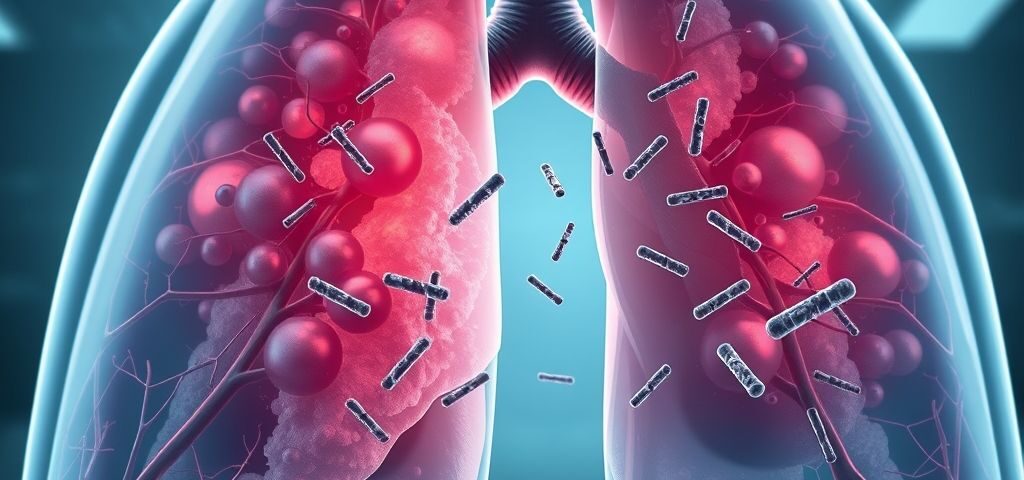
Legionnaires’ disease is a severe form of pneumonia caused by Legionella bacteria, primarily Legionella pneumophila. These bacteria thrive in warm water systems like cooling towers, hot tubs, plumbing systems, and air-conditioning units. When a person inhales small water droplets contaminated with Legionella, it can infect the lungs and lead to potentially life-threatening complications. Legionnaires Disease Treatment
Why It’s Still Relevant in 2025
Despite advancements in public health surveillance, Legionnaires’ disease remains a growing concern in 2025. Urbanization, climate change, and aging infrastructure have contributed to increased risks of outbreaks. Additionally, rising global travel and the continued use of large-scale water systems in hospitals, hotels, and public spaces increase exposure risk.
Public health agencies such as the CDC, WHO, and European Centre for Disease Prevention and Control (ECDC) have issued updated guidelines in 2025 to refine treatment protocols and reduce mortality rates.
Causes, Symptoms, and Diagnosis
Causes and Transmission
The disease is not spread from person to person. Instead, the bacteria are transmitted through:
Inhalation of aerosolized water droplets containing Legionella
Aspiration of contaminated water (especially in vulnerable patients)
Exposure to contaminated hot tubs, fountains, or HVAC systems
High-Risk Groups
In 2025, the most vulnerable populations include:
Adults over 50
Smokers and those with chronic lung disease
Immunocompromised individuals
Hospital patients, especially those in ICU settings
People with underlying conditions like diabetes or kidney disease
Common Symptoms
Symptoms typically appear 2–10 days after exposure and may include:
High fever (up to 104°F or 40°C)
Chills and muscle aches
Cough, which may bring up mucus or blood
Shortness of breath
Chest pain
Gastrointestinal symptoms (diarrhea, nausea)
Confusion or changes in mental status
These symptoms can rapidly progress, requiring urgent medical attention.
Diagnostic Approaches in 2025
Accurate diagnosis is critical for early intervention. Standard diagnostic tests include:
Urinary antigen test (UAT) – now widely used and refined for faster results in 2025
Sputum culture or bronchoalveolar lavage
PCR testing – used increasingly for high sensitivity
Chest X-ray or CT scan – to assess lung involvement
Legionnaires’ Disease Treatment Guidelines 2025
Overview of Updated Treatment Approach
The 2025 treatment guidelines reflect the need for early, targeted, and combination therapy for severe cases. The focus is on rapid diagnosis, effective antibiotics, supportive care, and post-treatment monitoring.
1. Antibiotic Therapy: First-Line Treatments
In 2025, the updated guidelines recommend macrolides and fluoroquinolones as the cornerstone of treatment:
a. Levofloxacin
Preferred fluoroquinolone
Dosage: 750 mg once daily for 7–10 days
Highly effective due to good lung penetration
b. Azithromycin
Macrolide of choice
Dosage: 500 mg IV or orally once daily
Often used in younger or less severe patients
c. New Addition: Omadacycline
Tetracycline-class antibiotic
Recommended in mild to moderate cases, especially in outpatient settings
Advantages include oral availability and broad-spectrum coverage
d. Combination Therapy
For severe pneumonia, ICU admission, or immunocompromised patients, dual therapy (e.g., levofloxacin + rifampin) may be used initially.
Route and Duration of Therapy
| Severity Level | Route of Administration | Duration |
| Mild/Moderate | Oral antibiotics | 7–10 days |
| Severe | IV antibiotics initially | 10–14 days |
| ICU patients | IV + combination therapy | 14–21 days |
Note: Step-down therapy from IV to oral is encouraged once the patient stabilizes.
Supportive Care Guidelines
In addition to antibiotics, supportive care plays a vital role:
Oxygen therapy for respiratory distress
Intravenous fluids for hydration
Mechanical ventilation in ICU settings
Antipyretics and pain relief medications
Nutritional support for prolonged illness
Hospitalization and Monitoring
Admission Criteria in 2025:
Patients should be hospitalized if they:
Have oxygen saturation < 90%
Exhibit altered mental status
Show radiologic evidence of multilobar pneumonia
Have significant comorbidities
Are immunocompromised
Monitoring Includes:
Daily clinical assessments
Blood tests (CRP, WBC, liver/kidney function)
Chest imaging to monitor progression
Follow-up urine antigen or PCR if relapse is suspected

Special Populations: Tailored Treatment
Elderly Patients:
Start with lower doses; monitor kidney function.
Avoid drug interactions with polypharmacy.
Immunocompromised:
Longer antibiotic duration (14–21 days).
Consider fungal or viral coinfections.
Outpatient Management in 2025
Select patients can be managed at home if:
Mild symptoms and stable vitals
No major comorbidities
Reliable follow-up is available
Outpatient treatment typically involves oral levofloxacin or azithromycin with monitoring every 48–72 hours.
Innovations in 2025: New Trends in Legionnaires’ Disease Management
AI-Powered Diagnostic Tools
Many hospitals now use AI-supported chest imaging software to differentiate Legionnaires’ disease from other types of pneumonia, speeding up decision-making.
Remote Monitoring Systems
For outpatient care, smart health apps and devices allow patients to monitor vitals and report symptoms, enabling early intervention if the condition worsens.

Environmental Surveillance Protocols
Updated regulations in 2025 require routine Legionella testing in water systems for:
Hospitals and nursing homes
Hotels and resorts
Commercial buildings with large HVAC systems
Preventive treatments include regular chlorination, heating systems maintenance, and automated water monitoring devices.
Advanced Clinical Management and Complications
Recognizing and Managing Complications in 2025
Even with timely treatment, Legionnaires’ disease can lead to complications, particularly in patients with pre-existing conditions or delayed diagnosis. The most common complications seen in 2025 include:
Septic shock
Acute respiratory distress syndrome (ARDS)
Renal failure (especially in elderly or diabetic patients)
Liver dysfunction
Neurological issues such as confusion or delirium
Management Strategies:
ICU Admission Criteria:
Persistent hypotension despite fluids
Multi-lobar pneumonia or bilateral infiltrates
Organ failure (renal, hepatic, respiratory)
Mechanical Ventilation:
Required for severe ARDS or respiratory failure, especially among elderly patients.
Hemodialysis:
Provided for acute kidney injury during the disease course.
Steroid Use in 2025:
Steroids are generally not recommended unless needed for another underlying condition, like COPD or adrenal insufficiency. They may mask symptoms or suppress the immune system.
Global and National Public Health Guidelines 2025
World Health Organization (WHO) Recommendations
The WHO 2025 policy update emphasizes:
Global Legionella Surveillance Systems (GLSS):
Implementation of real-time outbreak reporting systems globally.
Standardized Diagnostic Kits:
The 2025 model introduces rapid PCR-based point-of-care kits to detect Legionella within hours.
National Legislation Compliance:
Many countries now require mandatory Legionella testing in public and private infrastructure.
United States (CDC Guidelines 2025)
All healthcare facilities must implement a Water Management Program.
Mandatory reporting of cases to local health departments.
Use of electronic case reporting (eCR) systems integrated with hospital EMRs (electronic medical records).
European Union Guidelines 2025
Legionella Risk Assessment is mandated annually for hotels, spas, and public water systems.
Online Legionella Risk Registry to track buildings’ compliance in real time.

Environmental Control: Prevention is Better than a Cure
Guidelines for Facility Managers (Hospitals, Hotels, etc.)
In 2025, environmental control is a cornerstone of Legionnaires’ disease prevention. Updated standards now include:
Water Temperature Control:
Cold water ≤20°C
Hot water ≥60°C to kill Legionella
Regular Flushing of Systems:
Weekly or biweekly flushing of unused outlets (e.g., hospital wards or seasonal hotels).
Use of Copper-Silver Ionization Uni
Installed in major hospitals to eliminate Legionella in water tanks.
Smart Water Monitoring Devices:
IoT-based systems continuously monitor water quality and temperature.
Expert Quotes and Opinion in 2025
“Legionnaires’ disease is not just a clinical problem—it’s an environmental one. The 2025 guidelines reflect a shift toward integrated health and infrastructure safety.”
— Dr. Helena Marks, Infectious Disease Specialist, WHO
“What’s new in 2025 is the push for AI-powered diagnostics, which are game-changers for early identification and better outcomes.”
— Dr. Sean Riley, Director of Clinical Microbiology, Mayo Clinic
“We’ve reduced ICU stays by 20% this year by following the updated antibiotic protocols and implementing automated environmental surveillance.”
— Dr. Fatima Khan, Chief Medical Officer, NHS Hospital Trust
Legionnaires’ Disease and COVID-19 Co-infection Risks
Overlapping Symptoms in 2025
As COVID-19 continues to evolve with new variants, coinfections with Legionella are being documented more frequently. Overlapping symptoms such as cough, fever, and shortness of breath make diagnosis challenging.
Treatment Considerations
Dual Testing: All pneumonia patients in 2025 are advised to undergo dual testing for COVID-19 and Legionella.
Antibiotic Use: Antibiotics must be reserved for confirmed or highly suspected Legionnaires’ cases, not viral pneumonia.
Differentiation via AI tools: Chest imaging with machine learning software helps distinguish between viral and bacterial pneumonia.
Treatment, Recovery, and Rehabilitation
What to Expect After Recovery
Even after clearing the infection, many patients experience residual symptoms, especially if hospitalization was prolonged.
Common issues include:
Chronic fatigue
Decreased lung capacity
Mood changes or PTSD from ICU stays
Muscle weakness
Rehabilitation Programs in 2025
Most major hospitals now offer post-Legionnaires’ rehabilitation clinics, which include:
Pulmonary rehabilitation
Psychological support
Nutritional therapy
Gradual physical activity reintroduction
Patients are encouraged to undergo 3–6 months of follow-up after recovery to address long-term effects.
Conclusion: Key Takeaways for 2025
The 2025 guidelines for treating Legionnaires’ disease emphasize early diagnosis, appropriate antibiotic selection, and supportive care. With updated recommendations and better tools for environmental monitoring, public health agencies aim to reduce the morbidity and mortality associated with this preventable disease.
FAQs: Legionnaires’ Disease Treatment Guidelines 2025
1. What is the best antibiotic for Legionnaires’ disease in 2025?
Levofloxacin remains the first-line treatment due to its superior lung penetration and effectiveness. Azithromycin is also widely used, particularly for mild cases.
2. How long does treatment for Legionnaires’ disease last?
Treatment usually lasts between 7–14 days, depending on the severity and patient condition. ICU cases may require up to 21 days of therapy.
3. Can Legionnaires’ disease be treated at home?
Yes, if the case is mild and the patient is otherwise healthy. However, close follow-up is essential to ensure recovery.
4. Is there a vaccine for Legionnaires’ disease in 2025?
As of 2025, no approved vaccine exists. Research is ongoing, but prevention focuses on environmental control and rapid treatment.
5. What should be avoided during treatment?
Avoid unnecessary NSAIDs and corticosteroids unless prescribed. Also, avoid smoking and exposure to contaminated water sources.