Breathe deeply if you or a loved one has been diagnosed with ulcerative colitis (UC). We understand how overwhelming it is. Changes in lifestyle, medical costs, treatment options, and all the anxieties that can be like nightmares, but keep in mind, you are not the only one dealing with it. It’s important to understand UC in simple terms to manage it in a timely and better way.
What is Ulcerative Colitis?
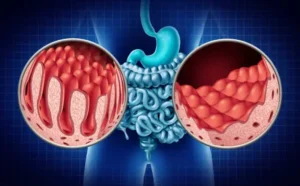
It is a long-term condition that is the cause of inflammation and ulcers (tiny sores) in the lining of your colon (large intestine) and rectum. It occurs when your body’s immune system becomes too out of control and attacks your digestive system.
It’s part of a group of conditions known as inflammatory bowel disease (IBD). Unlike other stomach issues, UC is not that easy to medicate, but don’t worry, it can still be managed with the proper care, suitable lifestyle changes, and full support.
Common Symptoms of Ulcerative Colitis
UC affects people in different ways, but many people experience these symptoms:
- Frequent, urgent usage of the bathroom: You might feel like you need to go even though you don’t need it.
- Cramping or pain in the abdomen: Usually in the lower left section of the abdomen.
- Diarrhea, often with blood or mucus
- Fatigue: Not just feeling tired, but bone-deep fatigue.
- Weight loss occurs as a result of improper nutrient absorption.
- Loss of appetite
- Fever (sometimes)
- Skin problems or joint pain (less common)
Symptoms can come and go; this is known as flare-ups and remission. During a flare-up, symptoms can get intense, and during remission, you might feel almost normal.
What Causes It?
Doctors and researchers are still working to figure out exactly why UC happens, but here’s what we know:
- Overactive immune response: Your immune system gets confused and attacks your colon, thinking it’s fighting off something harmful.
- Genetics: It often runs in families, so your chances are higher if a close relative has it.
- Environmental triggers: Certain infections, stress, or even diet changes might kickstart symptoms in people already prone to UC.
It’s not caused by stress or food alone, but both can affect how you feel and how often you flare.
Living with Ulcerative Colitis: How to Cope
Now, for the part that matters most, how do you live with UC without letting it control your life?
1. Find a doctor you trust
First things first: partner with a gastroenterologist (a stomach and intestine specialist) who listens to you and explains things in a way you understand. Good care starts with feeling seen and heard.
2. Medication is your ally, not your enemy
There’s no one-size-fits-all treatment, but medications can help reduce inflammation and keep symptoms under control. These can include anti-inflammatory drugs, immune system suppressors, and sometimes biologics (advanced medications that target specific parts of your immune system).
Taking your meds regularly, even when you feel fine, is key to avoiding flare-ups.
3. Keep a symptom journal
It doesn’t have to be fancy. Just jot down what you eat, how you feel, and how your digestion is doing each day. Patterns will start to appear. Maybe dairy makes things worse, or stress before a big event triggers symptoms. Knowing your triggers = power.
4. Watch your diet (but don’t obsess)
There’s no “UC diet” that works for everyone, but some foods tend to be easier on your gut:
- Soft, cooked veggies instead of raw
- Lean proteins (chicken, fish, tofu)
- White rice or potatoes
- Plain oatmeal
- Bone broth (gentle and nourishing)
During a flare-up, you might need to avoid high-fiber foods, dairy, caffeine, alcohol, or spicy foods.
Important: this doesn’t mean your diet has to be boring forever! Slowly reintroduce foods when you feel better, and always listen to your body.
5. Manage stress (because yes, it matters)
Stress doesn’t cause UC, but it can make it worse. Try things like:
- Deep breathing or meditation
- Gentle yoga or walking
- Journaling your thoughts
- Listening to calming music
- Talking to a therapist
Remember, mental health is physical health too.
6. Get support from people who get it
Talking to friends and family is great, but connecting with others who have UC can be deeply comforting. Whether it’s online forums, local support groups, or social media communities, sharing your experience with someone who understands makes a huge difference.
7. Prepare for public outings (just in case)
Let’s be real, knowing where the nearest bathroom is can be a lifesaver. Carry extra wipes, a change of underwear, or anything else that gives you peace of mind when you’re out and about. That doesn’t make you weak; it makes you smart and prepared.
8. Be kind to yourself
Living with UC is not your fault. You didn’t do anything to deserve this. Some days will be harder than others, and that’s okay. Celebrate the little victories, like a symptom-free day or finally figuring out which food was triggering your flare-ups.
Your journey won’t look like anyone else’s, and that’s perfectly fine.
When to Call Your Doctor
If you notice any of the following, don’t wait:
- Blood in your stool that’s getting worse
- Sudden weight loss
- Severe pain or cramping
- Fever
- Feeling faint or dizzy
Getting help early can prevent complications and give you more control over your health.
A Quick Word on Surgery
For some people, medications just aren’t enough. In that case, surgery to remove part or all of the colon may be considered. It sounds scary, but for many people, it brings relief and a better quality of life. If it comes to that, know that it’s not the end, just a new chapter.
Final Thoughts: You’ve Got This
Ulcerative colitis can change your life, but it doesn’t have to define it.
Yes, there will be tough days. But there will also be strong, beautiful, “I’ve got this” days. The more you understand your condition, the more empowered you’ll feel. And remember, managing UC isn’t about being perfect; it’s about finding your rhythm, getting support, and giving yourself grace.
You’re stronger than you think. And no matter where you are in your UC journey, know that you’re not alone. There’s a whole community out here walking this path with you.
Take care of yourself; you deserve it.
Frequently Asked Questions
- What causes ulcerative colitis?
Ulcerative colitis is caused by an overactive immune response that mistakenly attacks the colon lining. Genetics and environmental factors also play a role. - Can diet help manage ulcerative colitis?
While no specific diet cures UC, certain foods can reduce symptoms and prevent flare-ups. It’s important to identify and avoid your triggers. - Is ulcerative colitis curable?
There is currently no cure, but medications and lifestyle changes can help control symptoms and keep you in remission. - When should I see a doctor about my symptoms?
Seek medical help if you have severe abdominal pain, heavy bleeding, sudden weight loss, or persistent fever. - Can I live a normal life with ulcerative colitis?
Yes! With proper treatment, support, and self-care, many people with UC lead active, fulfilling lives.

