Clinical depression is more than just a fleeting feeling of sadness — it’s a serious mental health condition that affects how a person thinks, feels and functions in daily life. The early signs can be subtle, often mistaken for stress, burnout, or simply “having a bad week.” But left untreated, clinical depression can become debilitating and, in some cases, life-threatening. Early Signs of Clinical Depression
Recognizing the early signs of clinical depression can make a world of difference. The sooner someone receives the right support and treatment, the better their chances of recovery.
Understanding Clinical Depression
What Is Clinical Depression?
Clinical depression, also known as major depressive disorder (MDD), is a mental health condition characterized by persistent sadness, loss of interest in activities, and a range of emotional and physical problems. Unlike temporary mood dips, clinical depression lasts for at least two weeks — and often much longer — significantly affecting daily functioning.
It’s not about “snapping out of it” or “thinking positively.” Depression involves complex changes in brain chemistry, hormones, and neural pathways.
Clinical Depression vs. Feeling Sad
Feeling sad is a normal human emotion triggered by disappointments or challenges. It’s temporary and typically improves with time or a positive event.
Clinical depression, on the other hand:
Persists for weeks or months.
Disrupts work, relationships, and daily responsibilities.
Often occurs without a specific trigger.
Can lead to thoughts of self-harm or suicide.
How Common Is It?
According to the World Health Organization, depression affects over 280 million people worldwide. It’s one of the leading causes of disability globally, with women more commonly affected than men. However, men are less likely to seek help, which can lead to underdiagnosis.
Who Is Most at Risk?
Factors that increase the risk of clinical depression include:
A family history of depression or other mood disorders
Chronic illness or pain
Significant life stressors (loss of a job, divorce, bereavement)
History of trauma or abuse
Substance abuse
Hormonal changes (postpartum, menopause, thyroid issues)
What Are the Early Signs of Clinical Depression?
Early detection is critical because it allows for intervention before symptoms become overwhelming. Here’s what to watch for:
Persistent Sadness or Low Mood
A hallmark symptom, persistent sadness lingers for weeks, often without an obvious cause. It can feel like a heavy emotional fog that doesn’t lift.
Loss of Interest or Pleasure
Activities you once enjoyed — hobbies, social events, even favorite foods — may no longer bring joy. This is called anhedonia.
Changes in Appetite or Weight
Depression can cause significant changes in appetite, leading to unintended weight gain or loss. Some people overeat for comfort; others lose all desire to eat.
Sleep Disturbances
This can be insomnia (difficulty falling or staying asleep) or hypersomnia (sleeping excessively). Both worsen fatigue and mood.
Fatigue or Lack of Energy
Even small tasks, like showering or doing the dishes, can feel exhausting.
Difficulty Concentrating
Depression affects cognitive function, making it harder to focus, make decisions, or remember details.
Feelings of Guilt, Hopelessness, or Worthlessness
These thoughts can spiral into harmful beliefs about oneself, fueling the depression.
Physical Symptoms Without a Clear Cause
Headaches, digestive problems, and chronic pain can all be linked to depression.
Irritability or Restlessness
This is more common in men and teenagers, who may express depression through anger rather than sadness.
Social Withdrawal
Avoiding friends, family, and activities can be an early warning sign that depression is deepening.
Early Signs in Teenagers vs. Adults
Teens: more irritability, defiance, academic decline, withdrawal from peers.
Adults: more fatigue, pessimism, and workplace performance issues.
Early Signs in Men vs. Women
Men: more anger, substance use, physical complaints.
Women: more sadness, guilt, and anxiety symptoms.
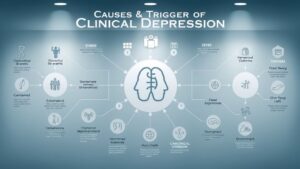
Causes & Triggers of Clinical Depression
Biological factors: neurotransmitter imbalances (serotonin, dopamine, norepinephrine)
Genetics: family history can increase risk
Hormonal changes: pregnancy, postpartum, menopause, thyroid problems
Trauma: abuse, loss, or major life changes
Chronic stress: work pressure, financial strain, caregiving burden
Medical conditions: chronic pain, heart disease, autoimmune disorders
Why Early Detection Matters
Better treatment outcomes: Early care can prevent severe episodes.
Reduced suicide risk: Prompt intervention can be life-saving.
Less disruption: Work, school, and relationships can be preserved.
Improved quality of life: More energy and emotional stability.
Treatment Options for Clinical Depression
Psychotherapy: Cognitive Behavioral Therapy (CBT), interpersonal therapy.
Medications: SSRIs (fluoxetine, sertraline), SNRIs, tricyclics, MAOIs.
Lifestyle changes: regular exercise, balanced diet, good sleep habits.
Alternative therapies: meditation, acupuncture, light therapy.
Clinical Depression Medication Side Effects
When starting antidepressants, many people experience side effects. These often improve within weeks, but awareness is key.
Common Side Effects:
Nausea, vomiting, diarrhea
Weight gain or loss
Dizziness or headaches
Dry mouth
Sexual dysfunction (low libido, difficulty reaching orgasm)
Serious (but rare) Side Effects:
Serotonin syndrome (confusion, fever, rapid heartbeat)
Suicidal thoughts in young adults
Allergic reactions (rash, swelling, difficulty breathing)
Managing Side Effects:
Take medication with food (if advised)
Adjust dosage with the doctor’s guidance
Report persistent or severe symptoms immediately
Never stop abruptly — taper under medical supervision
Coping Strategies & Self-Care Tips
Build a support network
Keep a daily routine
Set realistic goals
Practice mindfulness or meditation
Limit alcohol and avoid recreational drugs
Track mood changes in a journal
Supporting a Loved One with Clinical Depression
Listen without judgment
Avoid saying “Just cheer up.”
Offer to help with small tasks
Encourage professional treatment
Stay patient — recovery takes time

When to Seek Emergency Help
Seek immediate help if you notice:
Talking about wanting to die
Looking for means to self-harm
Expressing hopelessness or unbearable pain
Resources:
National Suicide Prevention Lifeline (US): 988
Samaritans (UK & Ireland): 116 123
Lifeline (Australia): 13 11 14
Real-Life Scenarios of Early Clinical Depression Signs
Sometimes reading a list of symptoms isn’t enough — seeing them in real-life contexts makes them easier to recognize.
Case Study 1: The Overworked Professional
Sana, 34, works in a competitive corporate environment. Over the past few months, she noticed she was constantly exhausted, struggling to meet deadlines, and avoiding after-work social events she once enjoyed. She began experiencing frequent headaches and waking up at 3 a.m. with racing thoughts.
At first, she assumed it was just stress. But when her appetite changed and she lost interest in hobbies, her friend suggested she speak to a therapist. She was later diagnosed with clinical depression, and starting treatment early helped her avoid a severe episode.
Case Study 2: The Withdrawn Teen
Hamza, 16, was once outgoing and athletic. For a semester, he stopped playing football, avoided friends, and spent most of his time in his room. His grades slipped, and he became irritable with family members.
His parents initially thought it was “just teenage moodiness,” but after a teacher reported he had been falling asleep in class and skipping meals, they sought professional help. Therapy and family support made a significant difference in his recovery.
Case Study 3: The Retired Caregiver
Imran, 68, cared for his wife during her long illness. After she passed away, he felt a deep emptiness. His days blurred together, and he stopped attending his community gatherings. Even activities like gardening, which once brought joy, no longer appealed to him.
His doctor recognized signs of clinical depression during a routine check-up and recommended counseling and a support group for widowed seniors. Gradually, his mood and energy improved.
Key takeaway: Clinical depression can appear differently depending on life stage, culture, and personality — but the common thread is a persistent change in mood, behavior, and physical well-being.
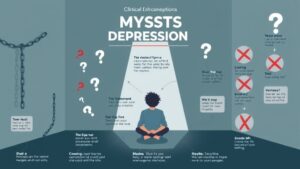
Myths and Misconceptions About Clinical Depression
Despite being one of the most common mental health conditions, clinical depression is still surrounded by myths that can prevent people from seeking help.
Myth 1: Depression is just sadness.
Reality: Depression is a medical condition that affects brain function, hormones, and physical health. It’s not something you can “snap out of.”
Myth 2: Only weak people get depressed.
Reality: Depression can affect anyone, regardless of strength, resilience, or achievements. It’s linked to biological, environmental, and social factors — not personal weakness.
Myth 3: Medication changes your personality.
Reality: Antidepressants aim to correct brain chemistry imbalances. When prescribed correctly, they help you feel more like yourself, not less.
Myth 4: Talking about depression makes it worse.
Reality: Discussing your feelings can reduce shame and lead to support and treatment. Avoiding the topic only prolongs suffering.
Preventing Clinical Depression Relapse
For many, depression is a recurring condition. Preventing relapse involves ongoing care and self-awareness.
Prevention strategies include:
Continuing therapy sessions even when feeling better
Taking medication as prescribed and discussing any changes with your doctor
Avoiding alcohol and drug misuse
Maintaining a balanced diet and regular exercise
Building strong social connections
Managing stress through relaxation techniques
How to Talk to Your Doctor About Depression
If you suspect you may have depression, preparing for your appointment can help you get the best care.
Before your visit:
Write down your symptoms, how long they’ve lasted, and any life changes or stressors.
Note any family history of depression or other mental illnesses.
List all medications and supplements you take.
Think about questions you want to ask, such as:
“What treatment options do you recommend?”
“What are the potential side effects of this medication?”
“How soon should I expect improvement?”
Lifestyle Habits That Support Recovery
While medical treatment is essential, healthy daily habits can boost recovery and improve mood.
- Regular Exercise
Physical activity releases endorphins — natural mood boosters. Even a 20-minute walk can make a difference. - Balanced Nutrition
Foods rich in omega-3 fatty acids, B vitamins, and antioxidants can support brain health. Examples: salmon, walnuts, spinach, blueberries. - Quality Sleep
Aim for 7–9 hours per night. Avoid caffeine after 2 p.m. and keep a consistent sleep schedule. - Mindfulness and Meditation
Mindfulness helps reduce stress and regulate emotions. Apps like Headspace or Calm can guide beginners. - Limiting Social Media
Constant comparison and negative news can fuel depressive thoughts—schedule “digital detox” times
Special Considerations: Depression During Pregnancy and Postpartum
Depression can occur during pregnancy (antenatal depression) and after childbirth (postpartum depression). Hormonal shifts, sleep deprivation, and lifestyle changes all contribute.
Early signs in postpartum women may include:
Persistent sadness or anxiety
Feeling disconnected from the baby
Difficulty bonding or feeling like an inadequate parent
Changes in sleep or appetite unrelated to newborn care
Treatment may involve:
Therapy (individual or group)
Safe medication under medical supervision
Support from family and community resources
The Link Between Chronic Illness and Depression
Chronic illnesses such as diabetes, heart disease, arthritis, and autoimmune disorders increase the risk of depression. The constant physical strain, medical costs, and lifestyle limitations can lead to feelings of hopelessness.
Tips for managing both conditions:
Coordinate care between your mental health provider and medical specialists
Stay physically active within your limits
Join support groups for your specific health condition

When Medication Isn’t Enough
For some, medication provides only partial relief. In such cases, other interventions may be considered:
Electroconvulsive Therapy (ECT): Used for severe, treatment-resistant depression
Transcranial Magnetic Stimulation (TMS): Uses magnetic fields to stimulate nerve cells in the brain
Ketamine Therapy: Administered under medical supervision for rapid symptom relief in some cases
These treatments are typically considered when other approaches haven’t worked.
Global Mental Health Resources
No matter where you live, help is available.
International Helplines:
Befrienders Worldwide: www.befrienders.org
Mental Health Europe: www.mhe-sme.org
World Health Organization – Mental Health: www.who.int/mental_health
Final Thoughts
Clinical depression is a medical condition that requires understanding, compassion, and proactive treatment. Recognizing the early signs of clinical depression — whether in yourself or a loved one — can be the first step toward recovery.
If you decide to take antidepressants, being informed about clinical depression medication side effects helps you navigate treatment more confidently. The journey may not be linear, but with the right support, therapy, and self-care, recovery is possible.
Conclusion
Recognizing the early signs of clinical depression can save lives. Whether it’s persistent sadness, loss of interest, or physical symptoms, early intervention offers the best chance for recovery.
If medication is part of the treatment plan, knowing the clinical depression medication side effects helps you make informed choices and work closely with your healthcare provider.
Depression is treatable, and recovery is possible — but it starts with recognizing the signs and reaching out for help.
FAQs
- What are the earliest warning signs of clinical depression?
Persistent sadness, loss of interest, fatigue, and changes in sleep or appetite are common early signs. - How is clinical depression diagnosed?
Through a clinical evaluation by a mental health professional, including symptom history and possible lab tests to rule out medical causes. - Can lifestyle changes help with clinical depression?
Yes. Exercise, a healthy diet, quality sleep, and stress management can all support recovery. - What are common side effects of antidepressants?
Nausea, dizziness, dry mouth, weight changes, and sexual side effects. - Do medication side effects go away over time?
Often they improve within a few weeks, but persistent or severe effects should be discussed with your doctor.